DRUGS ACTING ON
NERVOUS SYSTEM
PREPARED BY MR. ABHIJIT DAS
SEDATIVES AND
HYPNOTICS
Sedatives are a group
of drug that slow down brain activity without inducing sleep. These drugs are
prescribed to help patients calm down, feel more relaxed and get better sleep.
Hypnotics are a group
of drugs that induce sleep and reduce wakefulness during sleep.
Sedatives and hypnotics
are very commonly prescribed drugs because anxiety and
insomnia are very common problems.
Often, a drug which at
lower doses, produces sedation, causes hypnosis or even anaesthesia coma, and
death in sufficiently higher doses. For example barbiturates at lower doses
produce sedation, and at higher doses produce hypnosis.
ANXIETY
The person, without any
reason, develops an episode of panic which is
characterized by palpitation (rapid and irregular heart beat), fear of unknown,
sweating, dyspnea (shortness of breathing) etc.
INSOMNIA
The person take too much time after retiring into bed for falling asleep or
inability to stay in sleep that means the person’s sleep is broken repeatedly.
CLASSIFICATION:
BARBITURATES
LONG ACTING:
Phenobarbitone
SHORT ACTING:
Butobarbitone, Phentobarbitone
ULTRA-SHORT-ACTING:
Thiopentone, Methohexitone
BENZODIAZEPINES
HYPNOTIC: Diazepam,
Flurazepam, Nitrazepam, Alprazolam, Temazepam, Triazolam
ANTIANXIETY: Diazepam,
Chlordiazepoxide, Oxazepam, Lorazepam, Alprazolam
ANTICONVULSANT:
Diazepam, Lorazepam, Clonazepam, Clobazam
NEWER NONBENZODIAZEPIN
HYPNOTICS: Zopiclone, Zolpidem, Zaleplon
BARBITURATES:
MOA:
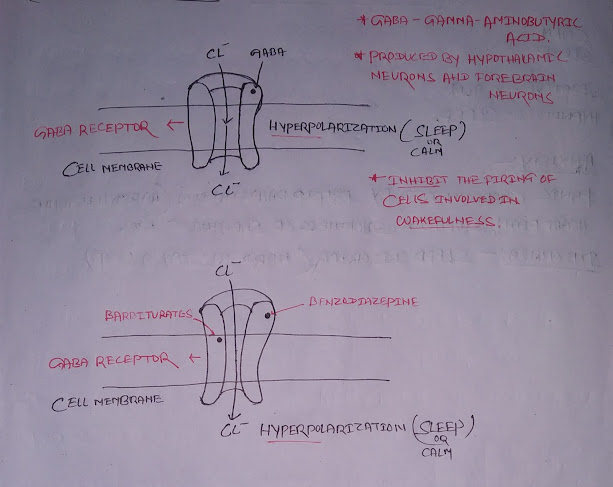
Barbiturates act by binding to GABA receptors, enhancing the inhibitory effect of
GABA neurotransmitter, which opens chloride
channels. This results in hyperpolarization
(No Depolarization) of neurons, leading to sedation and inhibition of neuronal
activity.
ADVERSE EFFECTS:
1.
Respiratory depression
2.
Dependence and tolerance
3.
CNS depression leading to drowsiness or
coma
4.
Hypotension
USES:
1.
Sedation/anesthesia induction
2.
Antiepileptic therapy
3.
Treatment of insomnia
BENZODIAZEPINES:
MOA:
Benzodiazepines act by binding to GABA receptors, enhancing the inhibitory effect of
GABA neurotransmitter, which opens chloride
channels. This results in hyperpolarization
(No Depolarization) of neurons and inhibition of neuronal activity.
ADVERSE EFFECTS:
1.
Drowsiness/fatigue
2.
Memory impairment
3.
Respiratory depression
4.
Dependence and withdrawal symptoms
USES:
1.
Anxiety disorders
2.
Insomnia
3.
Muscle relaxation
4.
Seizure disorders
ANTIDEPRESSANTS
Antidepressant drugs are medications prescribed to
help alleviate symptoms of depression and improve mood by influencing the
levels of certain chemicals in the brain called neurotransmitters.
CLASSIFICATION
1.
SELECTIVE SEROTONIN REUPTAKE INHIBITORS (SSRIS):
EXAMPLES:
Fluoxetine, Sertraline, Paroxetine, Escitalopram,
Citalopram.
MOA:
Selective Serotonin Reuptake Inhibitors (SSRIs) work
by blocking the reabsorption (reuptake) of serotonin in the brain. Serotonin is
a neurotransmitter, a chemical that helps transmit signals between nerve cells.
By inhibiting the reuptake of serotonin, SSRIs increase the concentration of
serotonin in the synapses (gaps between nerve cells), which can enhance
neurotransmission and alleviate symptoms of depression and anxiety. In simple
terms, SSRIs help keep more serotonin available in the brain, positively
affecting mood regulation.
ADVERSE EFFECTS:
a)
Insomnia
b)
Nausea
c)
Dry mouth
d)
Headache
USES:
a)
Depression
b)
Anxiety Disorders
c)
Panic Disorders
d)
Post-Traumatic Stress Disorder (PTSD)
2.
SEROTONIN-NOREPINEPHRINE REUPTAKE INHIBITORS (SNRIS):
EXAMPLES:
Venlafaxine, Duloxetine, Desvenlafaxine.
MOA:
Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs) work by blocking the reabsorption (reuptake) of both serotonin and norepinephrine in the brain, helping to increase the levels of these neurotransmitters. This enhanced presence of serotonin and norepinephrine in the synapses can positively impact mood and alleviate symptoms of depression and anxiety.
ADVERSE EFFECTS:
a)
Nausea
b)
Insomnia
c)
Increased Heart Rate
d)
Dry Mouth
e)
Dizziness
USES:
a)
Major Depressive Disorder
b)
Generalized Anxiety Disorder
c)
Chronic Pain Management
3.
MONOAMINE OXIDASE INHIBITORS (MAOIS):
EXAMPLES:
Amitriptyline, Nortriptyline, Imipramine, Doxepin,
Clomipramine.
MOA:
Monoamine Oxidase Inhibitors (MAOIs) work by
blocking the action of an enzyme called monoamine oxidase. This enzyme normally
breaks down neurotransmitters such as serotonin, norepinephrine, and dopamine.
By inhibiting monoamine oxidase, MAOIs increase the levels of these
neurotransmitters in the brain. This elevation in neurotransmitter levels can
help improve mood and alleviate symptoms of depression.
ADVERSE EFFECTS:
a)
Hypertensive Crisis (Severe Increase in
Blood Pressure)
b)
Weight Gain
c)
Drowsiness
d)
Dizziness
USES:
a)
Major Depressive Disorder
b)
Atypical Depression
c)
Social Anxiety Disorder
d)
Panic Disorder
SKELETAL MUSCLE
RELAXANTS
A centrally acting skeletal muscle relaxant is a
medication that targets the brain or spinal cord to reduce muscle contraction,
easing muscle spasms and stiffness.
CLASSIFICATION:
1.
GABAergic Agents:
·
Baclofen
·
Gabapentin
2.
Antispastic Agents:
·
Tizanidine
·
Diazepam (less common due to concerns
about tolerance and dependency)
BACLOFEN
MOA:
1.
Binding to GABA-B Receptors on
Upper Motor Neurons:
·
Baclofen binds to GABA-B receptors located on the terminals of upper motor neurons in the spinal cord.
·
This binding inhibits
the release of excitatory neurotransmitters such as glutamate by blocking
calcium (Ca++) channels.
·
By reducing the release of excitatory
neurotransmitters, baclofen decreases the excitability of upper motor neurons
and inhibits the signals that contribute to muscle spasticity.
2.
Binding to GABA-B Receptors on
Lower Motor Neurons:
·
Baclofen also binds to GABA-B receptors located on the soma (cell body)
of lower motor neurons.
·
This binding leads to the opening of potassium (K+) channels and subsequent efflux of potassium ions from the neuron.
·
The efflux of potassium ions
hyperpolarizes the neuron, making it less likely to reach the threshold for
depolarization and action potential firing.
·
By hyperpolarizing lower motor neurons,
baclofen further inhibits the transmission of signals to muscles, contributing
to muscle relaxation.
ADVERSE EFFECTS:
1.
Drowsiness
2.
Dizziness
3.
Weakness
4.
Fatigue
USES:
1.
Muscle spasms relief
2.
Treatment of muscle rigidity and pain
associated with certain neurological disorders.
TIZANIDINE
MOA:
- Tizanidine
binds to alpha2-adrenergic receptors
located on the terminals of upper motor neurons in the spinal cord.
- By binding to these receptors,
tizanidine
inhibits the release of excitatory neurotransmitters such as glutamate.
- This inhibition reduces the excitability of upper motor neurons and decreases the transmission of signals that contribute to muscle contraction.
ADVERSE EFFECTS:
1.
Drowsiness
2.
Dizziness
3.
Dry mouth
4.
Weakness
USES:
1.
Muscle spasticity relief
2.
Management of symptoms associated with
conditions such as multiple sclerosis or spinal cord injuries
ANTIPSYCHOTICS
Antipsychotics are medications primarily used to
manage symptoms of psychosis, which can include hallucinations, delusions, and
disordered thinking. They work by affecting certain neurotransmitters in the
brain to help alleviate these symptoms.
CLASSIFICATION:
1.
Typical (First-Generation)
Antipsychotics:
·
Examples: Chlorpromazine, Haloperidol,
Fluphenazine
2.
Atypical (Second-Generation)
Antipsychotics:
·
Examples: Risperidone, Olanzapine,
Quetiapine, Aripiprazole
TYPICAL ANTIPSYCHOTICS
MOA:
Typical (first-generation) antipsychotics work by blocking dopamine receptors in the brain, which
helps to reduce symptoms of psychosis like hallucinations and delusions.
ADVERSE EFFECTS:
1.
Drowsiness
2.
Dizziness
3.
Blurred vision
4.
Dry mouth
USES:
1.
Treatment of schizophrenia
2.
Management of acute psychotic episodes
3.
Control of agitation and aggression in
certain conditions
ATYPICAL ANTIPSYCHOTICS
MOA:
Atypical antipsychotics work by blocking dopamine and serotonin receptors in the brain, which
helps to reduce symptoms of psychosis.
ADVERSE EFFECTS:
1.
Drowsiness
2.
Dizziness
3.
Dry mouth
4.
Blurred vision
USES:
1.
Schizophrenia
2.
Acute psychotic episodes
3.
Agitation and aggression management
ANTIANXIETY DRUGS
Antianxiety drugs are medications used to alleviate
symptoms of anxiety disorders by calming the nervous system.
ANXIETY:
Anxiety is a natural response to stress or perceived
threats, but when it becomes chronic or overwhelming, it can be considered pathological
anxiety. Pathological anxiety involves excessive worry or fear that interferes
with daily life. It often involves a hyperactive
sympathetic nervous system, which is responsible for the body's
"fight or flight" response, leading to symptoms
like increased heart rate, sweating, and tremor.
CLASSIFICATION OF ANTIANXIETY DRUGS:
1.
SEDATIVES AND HYPNOTICS:
·
Examples:
Benzodiazepines (e.g., diazepam, lorazepam), Z-drugs (e.g., zolpidem, zaleplon)
·
Mechanism of Action (MOA):
Enhance the activity of the neurotransmitter gamma-aminobutyric acid (GABA) in
the brain, leading to a calming effect.
·
Adverse Effects:
Drowsiness, dizziness, confusion, risk of dependence and withdrawal symptoms
with long-term use.
·
Uses: Short-term
relief of anxiety, insomnia, and acute agitation.
2.
ANTIDEPRESSANTS:
·
Examples:
Selective Serotonin Reuptake Inhibitors (SSRIs) (e.g., sertraline,
escitalopram), Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs) (e.g.,
venlafaxine, duloxetine)
·
Mechanism of Action (MOA):
SSRIs increase serotonin levels in the brain, while SNRIs increase both
serotonin and norepinephrine levels, helping to regulate mood and reduce
anxiety.
·
Adverse Effects:
Nausea, headache, insomnia, increased risk of suicidal thoughts (especially in
young adults).
·
Uses:
Treatment of generalized anxiety disorder (GAD), panic disorder, social anxiety
disorder
3.
BETA BLOCKERS:
·
Examples:
Propranolol, atenolol
·
Mechanism of Action (MOA):
Block the effects of adrenaline (epinephrine) on beta-adrenergic receptors,
reducing the physical symptoms of anxiety such as rapid heartbeat, sweating and
trembling.
·
Adverse Effects:
Fatigue, dizziness, decreased heart rate, cold extremities.
·
Uses:
Management of performance anxiety (e.g., public speaking), treatment of
physical symptoms of anxiety such as palpitations and tremors.
ANTICONVULSANTS
Anticonvulsants are medications that help control or
prevent seizures, which are sudden,
uncontrolled electrical activity in the brain.
They work by stabilizing this abnormal activity,
reducing the likelihood of seizures occurring.
CLASSIFICATION:
1.
SODIUM CHANNEL BLOCKERS:
·
Examples:
Phenytoin, Carbamazepine, Lamotrigine.
·
MOA:
They block voltage-gated sodium channels,
reducing neuronal excitability and preventing the spread of abnormal electrical
activity.
·
Adverse Effects:
Possible adverse effects include dizziness, drowsiness, ataxia (loss of
coordination), and skin rash (especially with Lamotrigine).
·
Uses:
Treatment of epilepsy and bipolar disorder.
2.
CALCIUM CHANNEL BLOCKERS:
·
Examples:
Ethosuximide, Valproate.
·
MOA:
They block calcium channels, thereby
inhibiting neuronal activity.
·
Adverse Effects:
Adverse effects may include gastrointestinal disturbances, weight gain, liver
toxicity (especially with Valproate).
·
Uses:
Primarily used to treat seizures and
also used for mood stabilization (Valproate).
3.
GABA ENHANCERS:
·
Examples:
Benzodiazepines (e.g., Diazepam, Lorazepam), Barbiturates (e.g.,
Phenobarbital).
·
MOA:
They enhance the activity of gamma-aminobutyric
acid (GABA), which is an inhibitory
neurotransmitter, leading to activation chloride
(Cl-) channels (so, no
Depolarization).
·
Adverse Effects:
Adverse effects can include sedation, cognitive impairment, respiratory
depression (especially with high doses), and physical dependence.
·
Uses:
Acute (severe) seizure management (e.g., status epilepticus), adjunctive
therapy (or additional therapy) for various types of seizures.
4.
GLUTAMATE INHIBITORS:
·
Examples:
Topiramate, Felbamate.
·
MOA:
They inhibit glutamate release, reducing
excitatory neurotransmission.
·
Adverse Effects:
Potential adverse effects include cognitive impairment, weight loss, kidney
stones (especially with Topiramate)
·
Uses:
Treatment of epilepsy, including partial seizures.
5.
POTASSIUM CHANNEL OPENERS:
·
Examples:
Ezogabine (also known as Retigabine).
·
MOA:
They selectively activate potassium channels on
post synaptic neurons (so efflux of K+),
which can hyperpolarize neurons (no depolarization),
reducing their excitability.
·
Adverse Effects:
Adverse effects may include dizziness, urinary retention, and potential for
retinal abnormalities.
·
Uses:
Adjunctive (additional) treatment for partial seizures in adults.





.jpg)