URINARY SYSTEM
PREPARED BY MR. ABHIJIT DAS
INTRODUCTION
Ammonia, urea, uric acid, carbon dioxide, water and
ions are accumulated inside our body either by metabolic activities or by
excess ingestion. These substances have to be removed totally or partially from
our body.
Ammonia, urea and uric acid are the major
forms of nitrogenous wastes excreted by animals.
Humans along with many amphibians excrete urea and
are called ureotelic animals. The process
of elimination of urea is known as ureotelism.
The urinary system is the main excretory system in
humans. The urinary system plays a vital role in maintaining homeostasis of
water and electrolytes within the body.
The kidneys produce urine, which
contains metabolic waste products, including the nitrogenous
compounds such as urea and ammonia, excess ions and sometimes excreted drugs.
PARTS OF HUMAN URINARY SYSTEM
The urinary system is the main excretory system in
humans and consists of;
Ø Two
kidneys, which secrete urine.
Ø Two
ureters that pass the urine from the kidneys to the urinary bladder
Ø One
urinary bladder, which collects and stores urine
Ø One
urethra, through which urine leaves the body
Figure Credit: Jayashree Baidya
STRUCTURE OF KIDNEY
Kidneys are bean-shaped organs which
are reddish brown in colour.
Each kidney of an adult human measures 10-12cm in length, 5-7cm in
width and 2-3cm in thickness with an
average weight of 150g.
The kidneys lie on the dorsal
side of the abdominal wall, one on each side of the vertebral column.
There is a notch (depression)
towards the centre of the inner concave surface of the kidney called hilum through which urethra and blood vessels
enter.
The outer layer of the kidney is a tough capsule
made up of fats.
INTERNAL STRUCTURE OF KIDNEY
Inside the kidney, there are two zones, an outer cortex and
inner medulla.
The medulla is divided into few conical masses
called medullary pyramids.
The cortex extends in between the pyramids called
renal columns (or column of Bertini).
Urine formed within the kidney passes into the
drainage system that begins at a minor calyx (plural:
calyces). Several minor calyces merge into a major
calyx, and two or three major calyces combine to form a renal pelvis. The renal pelvis is a hollow funnel
shaped structure which leaves the kidney as ureter.
Figure Credit: Jayashree Baidya
FUNCTIONS OF KIDNEY
1.
Removal of Waste Materials:
·
The primary function of the kidneys is
to filter and remove waste products and excess fluids from the blood to form
urine.
2.
Removal of Drugs:
·
The kidneys play a crucial role in
filtering and eliminating drugs and their metabolites from the bloodstream.
3.
Secretion of Renin:
·
Renin is an enzyme that plays a key role
in regulating blood pressure and fluid balance in the body. The kidneys release
renin in response to various stimuli, such as low blood pressure or low sodium
levels.
4.
Secretion of Erythropoietin:
·
Erythropoietin is a hormone produced by
the kidneys in response to low oxygen levels in the blood. It stimulates the
bone marrow to produce more red blood cells.
NEPHRON
The structural and
functional unit of kidney is known as nephrons.
One kidney contains around 1 million nephrons.
Figure Credit: Jayashree Baidya
PARTS OF NEPHRON:
1.
Glomerulus:
·
A network of tiny blood vessels
(capillaries).
·
Receives blood from the afferent
arteriole and drains it through the efferent arteriole.
·
Site of blood filtration, where water,
ions, and small molecules are forced out of the blood into Bowman's capsule.
2.
Renal Tubule:
·
The renal tubule is a series of
connected tubular segments.
a. Bowman's Capsule (Glomerular Capsule):
·
A double-walled cup-shaped structure
surrounding the glomerulus.
·
Collects the filtered fluid (filtrate)
from the blood.
b. Proximal Convoluted Tubule (PCT):
·
The first segment of the renal tubule.
·
Site of reabsorption of
essential substances such as glucose, amino acids, and ions from the filtrate.
·
PCT is lined by simple
cuboidal brush border epithelium which increases the surface area for
reabsorption.
c. Loop of Henle (Nephron Loop):
·
Consists of a descending limb and an
ascending limb.
d. Distal Convoluted Tubule (DCT):
·
The segment following the loop of Henle.
·
Further reabsorption and secretion occur
here.
PHYSIOLOGY OF URINE FORMATION
There are three processes involved in the formation
of urine; glomerular filtration, tubular reabsorption and tubular secretion.
GLOMERULAR FILTRATION:
The first step in urine formation is the filtration
of blood by glomerulus which is called glomerular filtration.
The rate at which glomerular filtrate is being
formed is called glomerular filtration rate (GFR).
GFR in a healthy individual
is approximately 125ml/minute i.e. 180litres/day. Nearly all
(99%) of the filtrate is later reabsorbed from the kidney tubule to the
blood vessels. So, only 1-1.5 litres of
filtrate are excreted as urine.
The fluid filtered from the blood stream into the
glomerular capsule is now called filtrate and
it’s composition will be adjusted as it passes through the other parts of the
renal tubule.
Constituents of glomerular filtrates;
·
Water
·
Ions
·
Waste products
·
Glucose etc.
TUBULAR REABSORPTION:
- Essential substances such as water, glucose, amino acids, and ions are
reabsorbed from the renal tubule into the peritubular
capillaries (Peritubular capillaries are small blood vessels that
surround renal tubules in the kidneys) and returned to the bloodstream.
TUBULAR SECRETION:
Additional waste products,
certain drugs and excess ions are
actively secreted into the renal tubules from the peritubular capillaries,
enhancing their elimination from the body.
These processes collectively contribute to the
formation of urine, which is then transported the ureter, and stored in the
bladder until it is excreted from the body through the urethra.
RAAS (RENIN-ANGIOTENSIN-ALDOSTERON SYSTEM)
The primary aim of the Renin-Angiotensin-Aldosterone System (RAAS) is to regulate blood pressure and maintain fluid and
electrolyte balance in the body. The system is activated in response to various
stimuli, such as low blood pressure, low
sodium levels, or decreased blood volume.
STEPS OF RAAS:
1.
Blood Pressure Falls:
·
A decrease in blood pressure is
detected.
2.
Na+ Filtration Decreases:
·
Resulting in reduced sodium (Na+)
filtration in the kidneys.
3.
Fast Na+ Reabsorption:
·
Fast reabsorption of sodium occurs,
particularly in the distal convoluted tubule (DCT).
4.
DCT Detects Deficiency:
·
The distal convoluted tubule (DCT)
detects the sodium deficiency.
5.
Signaling to Afferent Arteriole:
·
The DCT releases signaling molecules
that act on the afferent arteriole.
6.
JG Cells Release Renin:
·
Juxtaglomerular (JG) cells of the
afferent arteriole release the enzyme renin.
7.
Renin Converts Angiotensinogen to
Angiotensin I:
·
Renin acts on angiotensinogen,
converting it into angiotensin I.
8.
ACE Converts Angiotensin I to
Angiotensin II:
·
Angiotensin I
is converted to angiotensin II by angiotensin-converting enzyme (ACE).
9.
Angiotensin II Actions:
·
Angiotensin II has three main actions:
·
Vasoconstriction:
Increases blood pressure by narrowing blood vessels.
·
Aldosterone (ADH)
Release: Promotes sodium and
water retention by the kidneys, which increases blood volume and blood
pressure.
·
Vasopressin (ADH)
Release: Enhances water
reabsorption, further increasing blood volume and pressure.
MICTURITION
Figure Credit: Jayashree Baidya
STEPS OF MICTURITION PROCESS:
1.
Stretch Receptors Activation:
·
The process begins with the filling of
the urinary bladder, causing its walls to stretch. Specialized stretch
receptors (mechanoreceptors) in the bladder wall detect this pressure.
2.
Sensory Signal to CNS:
·
The stretch receptors send sensory
signals to the central nervous system (CNS) indicating the level of bladder
fullness.
3.
Motor Signals to Bladder and
Sphincters:
·
The CNS sends two sets of motor signals:
·
Signal to the Bladder:
This signal stimulates the detrusor muscle of the
bladder to contract. The detrusor muscle contraction increases pressure
within the bladder, aiding in the expulsion of urine.
·
Signal to Internal Sphincter:
Another signal is sent to the internal sphincter
(smooth muscle), causing it to relax. The relaxation of the internal
sphincter facilitates the flow of urine from the bladder into the urethra.
4.
Voluntary Control with External
Sphincter:
·
This external sphincter surrounds the
urethra. The external sphincter allows for voluntary control over the
initiation or suppression of micturition.
KIDNEY FAILURE
Kidney failure, also known as renal failure, is a
medical condition where the kidneys are unable to adequately filter waste
products and excess fluids from the blood.
KIDNEY TRANSPLANT
A kidney transplant is a medical procedure in which
a healthy kidney from a living or deceased donor is surgically implanted into a
person with kidney failure.
GRAFT REJECTION:
Rejection of foreign organs by body’s immune system.
HEMODIALYSIS
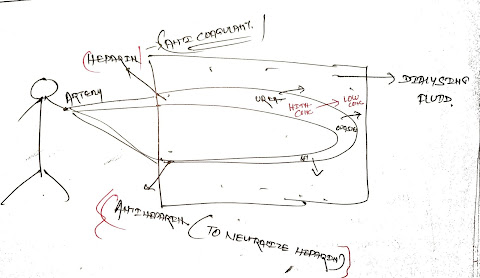
Ø
Hemodialysis
is a medical procedure used to filter waste products and excess fluids from the
blood when the kidneys are unable to perform this function adequately.
Ø During
hemodialysis, a machine (dialysis machine)
circulates the patient's blood through a special filter (dialyzer) to remove
waste and extra fluids before returning the cleansed blood to the body.
Ø Heparin is used in hemodialysis to prevent blood
clotting within the dialysis machine. Anti-heparin
agents may be administered to neutralize
heparin's anticoagulant effects if needed.
Ø Hemodialysis
is a vital treatment for individuals with advanced kidney disease or kidney
failure.
Ø A
common schedule for hemodialysis is typically three
times per week.
ABNORNAL URINE:
1. GLYCOSURIA:
sugar in urine
2. KETONURIA:
ketone bodies in urine
3. HEMATURIA: blood in urine
EASY TO REMEMBER