DRUGS ACTING ON
URINARY SYSTEM
PREPARED BY MR. ABHIJIT DAS
RAAS:
RAAS stands for the Renin-Angiotensin-Aldosterone
System, which is a crucial hormonal cascade involved in regulating blood
pressure and fluid balance.
1.
Renin:
Renin is an enzyme produced by the kidneys in response to various stimuli, such
as low blood pressure or decreased sodium levels. Renin acts on a precursor
protein called angiotensinogen, which is produced by the liver, to convert it
into angiotensin I.
2.
Angiotensin I to Angiotensin II:
Angiotensin I is converted into angiotensin II by the angiotensin-converting
enzyme (ACE), primarily found in the lungs.
3.
Vasoconstriction:
Angiotensin II is a potent vasoconstrictor, meaning it causes blood vessels to
narrow, leading to an increase in blood pressure.
4.
Aldosterone:
Angiotensin II also stimulates the release of aldosterone. Aldosterone is a
hormone produced by the adrenal glands. It acts on the DCT
and collecting tubule to increase the reabsorption of sodium (by
creating sodium potassium pumps) and water from the urine back into the bloodstream.
This process helps to retain sodium and water in the body, increasing blood
volume and blood pressure.
5.
Central Thirst System Activation:
Angiotensin II stimulates the central thirst mechanism in the brain, leading to
an increased sensation of thirst. This prompts individuals to drink more water, which can contribute to an increase in blood volume and subsequently elevate
blood pressure.
6.
Release of Vasopressin (ADH):
Angiotensin II also stimulates the release of vasopressin, also known as
antidiuretic hormone (ADH), from the pituitary
gland. Vasopressin acts on the DCT and
collecting tubule to promote water reabsorption, reducing urine output
and conserving water. This mechanism further contributes to an increase in
blood volume and helps maintain blood pressure.
DIURETICS:
Diuretics are drugs that increase urine production
in the body, aiding in the elimination of excess water and salt. They are
commonly prescribed to manage conditions such as hypertension, heart failure,
and edema.
CLASSIFICATION:
1.
Carbonic Anhydrase Inhibitors:
·
Example: Acetazolamide
2.
Loop Diuretics:
·
Examples: Furosemide, Bumetanide,
Torsemide
3.
Thiazide Diuretics:
·
Examples: Hydrochlorothiazide,
Chlorthalidone, Indapamide
4.
Potassium-Sparing Diuretics:
·
Examples:
·
Aldosterone Antagonists: Spironolactone,
Eplerenone
·
Non-aldosterone Antagonists: Amiloride,
Triamterene
5.
Osmotic Diuretics:
·
Examples: Mannitol, Glycerin
CARBONIC ANHYDRASE INHIBITORS:
MOA:
Carbonic anhydrase inhibitor works by blocking an enzyme called carbonic anhydrase in
the proximal convoluted tubule (PCT) of the
kidney. By doing this, it helps more sodium ions
(Na+) to be flushed out in the urine. When there's more
sodium in the urine, it pulls more water along with it from the nephron,
leading to increased urine production.
ADVERSE EFFECTS:
1.
Acid Buildup:
Can cause body acidity, leading to confusion and rapid breathing.
2.
Electrolyte Problems:
Imbalance in minerals like sodium can cause weakness and irregular heartbeat.
USES:
1.
Glaucoma:
Helps reduce pressure inside the eye by decreasing the production of aqueous
humor, easing symptoms like eye pain and vision problems.
2.
Edema and Hypertension:
Helps to reduce swelling and lower blood pressure by increasing the removal of
excess fluid and sodium through urine.
3.
High Altitude Sickness:
Can alleviate symptoms of altitude sickness by stimulating breathing and
improving oxygen levels in the blood.
LOOP DIURETICS:
MOA:
Loop diuretics inhibit
the sodium-potassium-chloride cotransporter (Na+K+2Cl-)
in the thick ascending limb of the loop of Henle in the kidney,
preventing reabsorption of sodium, potassium, and chloride ions. This leads to
increased excretion of these ions in urine, along with water, causing diuresis.
ADVERSE EFFECTS:
1.
Electrolyte Imbalance:
Can lead to low levels of potassium, sodium, and chloride, causing weakness and
irregular heartbeat.
2.
Dehydration:
Excessive urination may cause dry mouth, thirst, and dizziness.
3.
Hypotension:
May result in low blood pressure, leading to lightheadedness and fainting.
USES:
1.
Edema:
Used to reduce swelling caused by conditions like heart failure or kidney
disease.
2.
Hypertension:
Helps lower blood pressure by decreasing fluid volume in the body.
THIAZIDE DIURETICS:
MOA:
Thiazide diuretics work primarily by inhibiting the sodium-chloride cotransporter (Na+Cl-
Cotransporter) in the distal convoluted tubule (DCT) of the kidney. By doing
so, they decrease the reabsorption of sodium
and chloride ions, leading to increased excretion of these ions in the urine. This
results in diuresis.
ADVERSE EFFECTS:
1.
Electrolyte Imbalance:
Can cause low sodium levels, leading to weakness and irregular heartbeat.
Kaliuresis exacerbates potassium loss.
2.
Hyperglycemia:
May raise blood sugar levels, especially in people with diabetes.
3.
Hyperuricemia and Gout:
Can increase uric acid levels, triggering or worsening gout attacks in some
individuals.
USES:
1.
Edema:
Helps reduce swelling caused by conditions like heart failure or kidney
disease.
2.
Hypertension:
Lowers blood pressure by reducing fluid volume in the body.
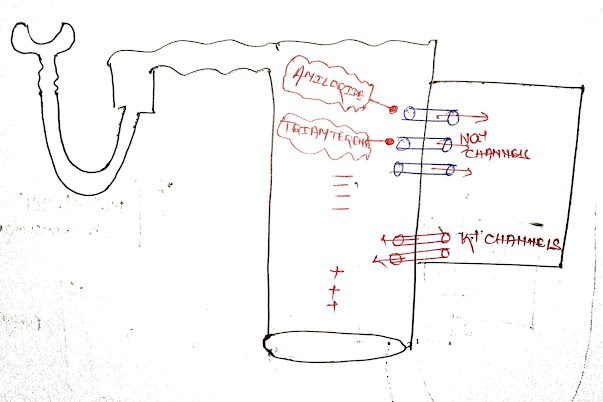
POTASSIUM-SPARING DIURETICS:
MOA:
Potassium-sparing diuretics work by blocking the sodium channels in the distal convoluted
tubule (DCT) and collecting ducts of the kidney. This action prevents the reabsorption of sodium ions, leading to
increased excretion of sodium in the urine.
ADVERSE EFFECTS:
1.
High Potassium:
These diuretics can raise potassium levels in the blood, causing muscle
weakness, irregular heartbeats, and dangerous heart rhythm issues.
2.
Acid-Base Imbalance:
Sometimes they can upset the body's acid-base balance, leading to confusion,
fatigue, and rapid breathing.
USES:
1.
Heart Failure:
Potassium-sparing diuretics are often used in the management of heart failure
to help reduce fluid buildup and ease the workload on the heart.
2.
Hypertension:
They can be used as part of a treatment plan for high blood pressure, helping
to lower blood pressure without causing potassium loss.
3.
Hypokalemia Prevention:
In some cases, they may be prescribed alongside other diuretics to counteract
potassium loss and prevent hypokalemia (low potassium levels).
OSMOTIC DIURETICS:
MOA:
Osmotic diuretics work primarily by increasing the osmotic pressure in the renal
tubules, specifically in the proximal convoluted tubule and descending loop of
Henle. This prevents the reabsorption of water,
leading to increased urine production.
ADVERSE EFFECTS:
1.
Dehydration:
Excessive urine production caused by osmotic diuretics can lead to dehydration,
which may manifest as symptoms such as dry mouth, thirst, decreased urine
output, and dizziness.
2.
Electrolyte Imbalance:
Osmotic diuretics can disrupt the balance of electrolytes such as sodium and
potassium, leading to abnormalities in the body's electrolyte levels. This
imbalance can result in symptoms like weakness, muscle cramps, and irregular
heartbeat.
USES:
1.
Cerebral Edema:
Reduces brain swelling in conditions like head injuries or strokes.
2.
Acute Kidney Injury:
Helps improve kidney function by increasing urine output.
3.
Glaucoma:
Lowers pressure in the eyes during certain eye conditions or surgeries.
ANTIDIURETIC DRUGS
DEFINITION
Antidiuretic drugs, also known as vasopressin or
antidiuretic hormone (ADH) agonists, are medications that mimic the action of
vasopressin in the body. Vasopressin is a hormone produced by the hypothalamus
and released from the posterior pituitary gland. Its primary function is to
regulate water balance in the body by controlling the reabsorption of water in
the kidneys. Antidiuretic drugs are used to treat conditions characterized by
excessive urination and water loss, such as diabetes insipidus.
CLASSIFICATION OF ANTIDIURETIC DRUGS:
1.
Synthetic Vasopressin Analogues:
·
Desmopressin (DDAVP): Used for diabetes
insipidus, nocturnal enuresis (bedwetting), and certain bleeding disorders like
hemophilia.
2.
Vasopressin Receptor Agonists:
·
Conivaptan: Used in hospitalized
patients to manage hyponatremia (low sodium levels).
·
Tolvaptan: Used to treat hyponatremia
associated with heart failure and certain other conditions.
MECHANISM OF ACTION OF VASOPRESSIN
Vasopressin acts on V2 receptors in the DCT and
Collecting Tubule of the kidney, increasing water permeability. This leads to
water reabsorption and concentrated urine.
ADVERSE EFFECTS OF ANTIDIURETIC DRUGS:
1.
Fluid Retention: Excessive use or
improper dosage of antidiuretic drugs can cause fluid retention, leading to
edema (swelling) and potential cardiovascular complications.
2.
Headache: Some individuals may
experience headaches as a side effect of antidiuretic drugs.
3.
Gastrointestinal Disturbances: Nausea,
vomiting, and abdominal cramps may occur in some cases.
4.
Hypertension: In certain situations,
antidiuretic drugs may cause an increase in blood pressure.
THERAPEUTIC USES OF ANTIDIURETIC DRUGS:
1.
Diabetes Insipidus: Antidiuretic drugs,
particularly desmopressin, are the primary treatment for central diabetes
insipidus, a condition characterized by excessive thirst and urination due to
inadequate vasopressin secretion.
2.
Nocturnal Enuresis: Desmopressin nasal
spray is used to treat bedwetting in children and adults.
3. Hyponatremia: Vasopressin receptor antagonists like tolvaptan and conivaptan are used in certain cases of hyponatremia to raise sodium levels.
URINARY ANTISEPTICS:
Urinary antiseptics are medications used to treat
urinary tract infections (UTIs) by preventing the growth of bacteria in the
urinary system. These medications work by either directly killing bacteria or
by inhibiting their growth.
Some common urinary antiseptics include:
NITROFURANTOIN
MOA:
Nitrofurantoin inhibits bacterial DNA synthesis by inhibiting DNA gyrase, an enzyme crucial for
DNA replication and repair, ultimately leading to bacterial cell death.
METHENAMINE
MOA:
Methenamine, when metabolized in the acidic
environment of the urinary tract, releases
formaldehyde. Formaldehyde damages bacterial
cell membranes, disrupting their structure and function, ultimately
leading to bacterial cell death.
TRIMETHOPRIM-SULFAMETHOXAZOLE
MOA:
Trimethoprim-sulfamethoxazole inhibits bacterial
growth by blocking two consecutive steps in the folate synthesis pathway: sulfamethoxazole inhibits dihydropteroate synthase, while
trimethoprim inhibits dihydrofolate reductase, collectively
preventing the production of essential folate
derivatives needed for bacterial DNA synthesis.
TREATMENT OF UTI-ACIDIFIERS AND ALKALINIZERS:
ACIDIFIERS:
Acidifiers work by increasing
the acidity of urine, creating an environment less favourable to the growth of
certain bacteria.
Examples of acidifying agents indeed include ascorbic acid (vitamin C) and cranberry supplements.
ALKALINIZERS:
Alkalinizers work by increasing the alkalinity of
urine, which can help alleviate symptoms such as a burning sensation during
urination.
Examples: Potassium citrate and sodium bicarbonate
are commonly used as alkalinizing agents in the treatment of urinary tract
symptoms associated with acidic urine.